Foot & Ankle
Foot and ankle injuries can be complex and debilitating. Bone & Joint Specialists of Winchester Specialists provide comprehensive care, including diagnosis, treatment and rehabilitation for all types of foot and ankle problems. We provide care for patients of all ages, listening and working together to customize the right treatment plan, whether for bunions, fractures or complex neuromuscular disorders.
Examples of conditions treated by a foot and ankle surgeon are:
- Bunions
- Hammertoes
- Sports injuries
- Trauma of the foot and ankle
- Reconstructive procedures
- Plantar fasciitis and heel spur syndrome
If you have pain in your foot or ankle or any of the conditions listed above, you should consult an orthopaedic foot and ankle specialist.
CAO serves patients in Virginia, West Virginia, Washington D.C., and Maryland.
Common Podiatry Conditions and Procedures
Patients come to Bone & Joint Specialists of Winchester's Joint Replacement Physicians seeking long-term relief from arthritis, injury and overuse. Podiatrists can perform surgery, reset broken bones, prescribe drugs, and order lab tests or X-rays. They can also help with general foot care, such as picking the correct shoe size, obtaining footwear inserts or orthotics, and suggesting stretches or exercises.
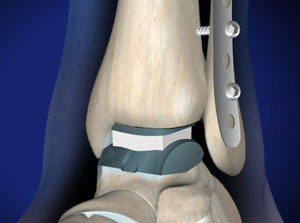
 The surgeons at Bone and Joint Specialists of Winchester are experts in the comprehensive care of ankle fractures. Dr. Golding in particular specializes in fractures of the foot and ankle. It can be frightening to try and manage an injury like this. So, let's dive into this problem together; exploring what they are, how non-surgical treatments work for simple fractures, when surgery is necessary, and what to expect during the recovery journey.
The surgeons at Bone and Joint Specialists of Winchester are experts in the comprehensive care of ankle fractures. Dr. Golding in particular specializes in fractures of the foot and ankle. It can be frightening to try and manage an injury like this. So, let's dive into this problem together; exploring what they are, how non-surgical treatments work for simple fractures, when surgery is necessary, and what to expect during the recovery journey.
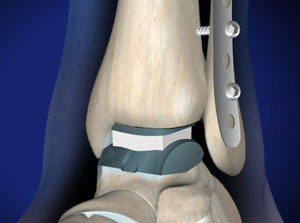
An ankle fracture occurs when one or more bones that make up the ankle joint break. This can happen due to a variety of reasons, such as a fall, sports injury, or a sudden twist. Ankle fractures are common, but the good news is that with the right care, they can heal well, restoring stability and function.
The primary goal of ankle fracture treatment is to allow the bones to heal in their proper position and to manage pain. If the broken bones are out of position, surgery may be needed to properly align the fragments of bone and then hold them in position so they heal well.
But not all ankle fractures require surgery. Simple fractures, where the bones are not out of place, can often be treated without surgery. Here's how it's typically done:
-
Immobilization: A cast or a brace may be applied to keep the ankle in a stable position, allowing the bones to mend.
-
Rest and Elevation: Resting the affected ankle and keeping it elevated helps reduce swelling and promotes healing.
-
Pain Management: Over-the-counter pain medications or prescribed pain relievers may be recommended to manage discomfort.
-
Physical Therapy: As healing progresses, gentle exercises may be introduced to restore strength and flexibility.
By opting for non-surgical treatment, we aim to provide effective care while minimizing disruption to your daily life.
Certain ankle fractures are more complex, requiring surgical intervention to ensure optimal healing. These may include fractures where the bones are significantly displaced, or involve joint surfaces, or maybe ones that have associated ligament injuries. As ankle fracture specialists, our expertise lies in evaluating the specific characteristics of the fracture to determine the most appropriate course of action.
Selecting a podiatric or orthopedic surgeon with expertise in ankle fractures ensures that you receive personalized care tailored to your unique situation. We prioritize precision and individualized treatment plans. Our goal is to guide you through the process, offering both medical expertise and compassionate support.
Recovering from ankle fracture surgery is a gradual process, and each patient's journey is unique. But here's a general overview of what to expect:
- Immediate Post-Surgery Period: You may need crutches or a walker to move around, and keeping weight off the operated ankle is essential. This period usually lasts 6-12 weeks.
- Follow-Up Appointments: Regular check-ups are crucial to monitor healing progress and make any necessary adjustments to the treatment plan.
- Physical Therapy: A structured physical therapy program will be initiated to regain strength, flexibility, and functionality in the ankle. This will usually start when the fracture is adequately healed to allow motion and strengthening.
- Gradual Return to Activities: As healing advances, you'll gradually increase weight-bearing on the operated ankle and resume daily activities.
- Monitoring Long-Term Healing: Follow-up appointments will continue to ensure the long-term success of the treatment. If you have plates and screws placed during surgery, these are often designed to remain in place for your lifetime. But in some cases, they are designed to be temporary and may need to be removed.
By choosing an ankle fracture specialist, you're investing in expert care that prioritizes your well-being throughout the recovery
Ankle fractures are manageable with the right expertise and care. As your dedicated ankle fracture specialist, we are committed to providing comprehensive and compassionate treatment, guiding you towards a swift and successful recovery. If you're seeking an experienced professional for your ankle fracture, look no further—your journey to healing starts here. Learn more about Dr. Stephanie Golding at Bone and Joint Specialists of Winchester today for expert care and effective treatments. Get back to walking comfortably and confidently!
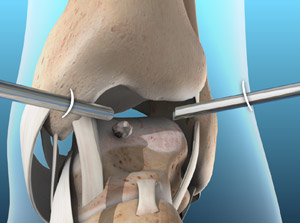
 Ankle sprains are very common. And repeated sprains can make you prone to future injuries. In some cases, repeated sprains can damage the ankle ligaments permanently and require a specialists’ attention to fix chronic ankle instability. Dr. Golding is specially trained in the most cutting-edge ways to manage ankle sprains and instability and getting you back to enjoying life. Let's explore the realm of ankle injuries together. This article will discuss what ankle sprains are, how non-surgical treatments work for simple sprains, when surgery becomes necessary for chronic instability, and the expected recovery journey.
Ankle sprains are very common. And repeated sprains can make you prone to future injuries. In some cases, repeated sprains can damage the ankle ligaments permanently and require a specialists’ attention to fix chronic ankle instability. Dr. Golding is specially trained in the most cutting-edge ways to manage ankle sprains and instability and getting you back to enjoying life. Let's explore the realm of ankle injuries together. This article will discuss what ankle sprains are, how non-surgical treatments work for simple sprains, when surgery becomes necessary for chronic instability, and the expected recovery journey.
Ankle sprains occur when the ligaments (which are tough bands of tissue connecting the ankle bones) become stretched or torn. This often happens due to a sudden twist or turn, leading to pain, swelling, and difficulty moving the ankle. Whether you're an athlete or simply navigating everyday activities, ankle sprains can happen to anyone. Our first goal is to check whether or not the ankle is just sprained or broken, which usually requires x-rays. We make take additional specialized x-rays to look for uncommon fractures that might be missed on basic films.
Simple ankle sprains, where the ligaments are mildly injured, can often be effectively treated without surgery. Our approach to non-surgical treatments is tailored to each patient's unique needs:
-
Rest and Ice: Adequate rest and applying ice help reduce swelling and promote healing in the early stages.
-
Compression and Elevation: Wrapping the ankle and keeping it elevated further aid in minimizing swelling and supporting the healing process.
-
Pain Management: Over-the-counter or prescribed pain relievers may be recommended to manage pain during the recovery period.
-
Physical Therapy: Targeted exercises are introduced to restore strength, stability, and flexibility in the ankle.
With a focus on personalized care, non-surgical treatments aim to facilitate a smooth recovery and prevent future issues.
While many ankle sprains heal well with conservative measures, some individuals may experience chronic instability, characterized by repeated sprains and a feeling of unsteadiness. Surgical intervention may be considered in cases of severe ligament damage or persistent instability. As a specialist in ankle sprains and chronic instability, we assess each patient comprehensively to determine the most suitable treatment plan.
Opting for a specialist with expertise in ankle sprains ensures that you receive cutting-edge care designed to address the root cause of your symptoms with the most modern techniques. These may include ligament repairs or reconstructions to provide long-term restoration of function and the stability you need to hike, ride, and play.
Recovering from surgical intervention for chronic ankle instability involves a phased approach:
-
Post-Surgery Period: Initially, you may need to use crutches or a brace to support the healing process.
-
Follow-Up Appointments: Regular check-ups are crucial to monitor healing progress and address any concerns.
-
Physical Therapy: A tailored physical therapy program is initiated to enhance strength, stability, and overall ankle function.
-
Gradual Resumption of Activities: As healing progresses, you'll gradually resume weight-bearing activities under guidance.
-
Long-Term Monitoring: Follow-up appointments continue to monitor long-term healing and address any potential issues.
By selecting an ankle sprain specialist, you're choosing expert care that prioritizes your comfort and well-being throughout the recovery process.
Ankle sprains and chronic instability are manageable with the right expertise and care. As your dedicated ankle sprain specialists, we are committed to providing comprehensive and compassionate treatment, guiding you towards lasting relief. If you're seeking an experienced professional for your ankle sprain or chronic instability, your path to recovery begins here.
Learn more about Dr. Stephanie Golding at Bone and Joint Specialists of Winchester today for expert care and effective treatments. Get back to walking comfortably and confidently!
 Many people have questions about bunions - a common yet often misunderstood foot condition. This article will help you understand what bunions are, how your family history plays a role in developing bunions, various non-surgical treatments, and when surgical intervention might be needed. We will also talk about postoperative care and recovery. This comprehensive guide aims to provide you with expert insights into bunions and their management. Here at Bone and Joint Specialists of Winchester, Dr. Golding provides expert management for bunions of all kinds.
Many people have questions about bunions - a common yet often misunderstood foot condition. This article will help you understand what bunions are, how your family history plays a role in developing bunions, various non-surgical treatments, and when surgical intervention might be needed. We will also talk about postoperative care and recovery. This comprehensive guide aims to provide you with expert insights into bunions and their management. Here at Bone and Joint Specialists of Winchester, Dr. Golding provides expert management for bunions of all kinds.
Bunions, medically known as hallux valgus, are bony bumps that develop on the joint at the base of the big toe. This condition is caused by the big toe angling towards the second toe, leading to a noticeable and painful bump on the inside of the foot. The prominence of the bunion can result in pain, swelling, and difficulty finding comfortable shoes.
Several factors contribute to the development of bunions, with the primary one being genetics. People with inherited foot issues are more prone to bunions due to the way their bones and joints are aligned and how flexible their ligaments are. Additionally, wearing ill-fitting shoes, especially those with narrow toe boxes, high heels, or pointed toes, can exacerbate the condition. Other factors, such as arthritis and foot injuries, may also contribute to bunion formation.
Yes, bunions can be familial. If your parents or grandparents had bunions, you may be more predisposed to develop them. While genetics play a significant role, environmental factors like footwear choices and certain activities can influence the severity and progression of bunions. If bunions run in your family, proactive measures, and early intervention can help manage and alleviate potential issues.
Non-surgical treatments for bunions focus on relieving symptoms and slowing down the progression of the condition. I often recommend the following approaches:
- Footwear Modifications: Wearing shoes with a wide toe box and low heels can reduce pressure on the bunion and alleviate discomfort.
- Orthotic Devices: Custom-made orthotics provide support and help distribute pressure more evenly across the foot.
- Padding and Taping: Applying pads or tape to the bunion can alleviate friction and pressure, reducing pain.
- Anti-Inflammatory Medications: Non-prescription medications like ibuprofen can help manage pain and inflammation.
- Physical Therapy: Specific exercises can improve joint flexibility and strengthen muscles around the affected area.
Early and consistent application of these non-surgical measures can effectively manage bunions and improve overall foot comfort.
When non-surgical methods are insufficient, surgical intervention may be considered to correct bunions. Common surgical procedures include:
- Bunionectomy: This involves removing the bony bump and realigning the toe joint.
- Osteotomy: The surgeon cuts and realigns the bone to correct the toe's angle.
- Arthrodesis: This fuses the joint to provide stability and reduce pain.
The choice of surgery depends on the severity of the bunion, the extent of joint damage, and individual patient factors.
Recovery time varies depending on the type of surgery performed. Generally, patients can expect:
- First Few Weeks: Limited or non-weightbearing and the use of crutches or a special shoe. Some people may be allowed to bear weight on the heel of the foot while protecting the toes from weight.
- Several Weeks After Surgery: Gradual resumption of normal activities under the guidance of the surgeon and therapist.
- Full Recovery: Complete healing may take several months, and return to regular shoes may occur gradually. Feet heal more slowly than other parts of the body and scar tissue may be sore for a longer period of time than in other parts of the body.
Following postoperative care instructions, attending follow-up appointments, and adhering to recommended activity restrictions are crucial for a successful recovery.
Yes, patients can walk after bunion surgery, but it's typically a gradual process. The initial recovery phase involves limited or non-weightbearing depending on the procedure performed, and patients may use crutches or a special shoe to protect the foot. As healing progresses, the surgeon will guide patients on gradually increasing weight-bearing activities. Returning to normal walking and footwear usually occurs as the foot heals and gains strength.
In the realm of bunions, a balance of expertise and compassionate care is key to effective management. As a foot surgeon committed to foot health, Dr. Golding advocates for early intervention, personalized treatment plans, and comprehensive postoperative care. Whether exploring non-surgical options or considering surgical intervention, rest assured that expert guidance is available to help you navigate the path to relief and improved foot health. If you're dealing with bunions, remember, you're not alone—let's take the journey to healthier, happier feet together!
A balance of expertise and compassionate care is key to effective bunion management. As a foot surgeon committed to foot health, Dr. Golding advocates for early intervention, personalized treatment plans, and comprehensive postoperative care. Whether exploring non-surgical options or considering surgical intervention, rest assured that expert guidance is available to help you navigate the path to relief and improved foot health. If you're dealing with bunions, remember, you're not alone—let's take the journey to healthier, happier feet together!
Learn more about Dr. Stephanie Golding at Bone and Joint Specialists of Winchester today for expert care and effective treatments.
 Flat feet are a common condition that can greatly affect one's quality of life. From understanding what flatfoot is to exploring familial connections, non-surgical treatments, and surgical interventions, this comprehensive guide aims to provide expert insights into flatfoot deformity and its multifaceted management. Here at Bone and Joint Specialists of Winchester, Dr. Stephanie Golding is our expert in treating flatfoot deformities.
Flat feet are a common condition that can greatly affect one's quality of life. From understanding what flatfoot is to exploring familial connections, non-surgical treatments, and surgical interventions, this comprehensive guide aims to provide expert insights into flatfoot deformity and its multifaceted management. Here at Bone and Joint Specialists of Winchester, Dr. Stephanie Golding is our expert in treating flatfoot deformities.
Flatfoot deformity, also known as pes planus, occurs when the arch of the foot collapses, causing the entire sole to touch the ground. This condition can be flexible, with the arch appearing when the foot is off the ground. Or it can be rigid, where the arch remains flattened in all positions. Flatfoot deformity can lead to pain, swelling, and difficulty with everyday activities.
Flatfoot deformity can arise from a variety of factors, both genetic and environmental. While some individuals inherit a foot structure predisposed to flatfoot, other contributing factors include obesity, injury, arthritis, and certain systemic conditions. In particular, posterior tibial tendon dysfunction (PTTD) plays a crucial role in the development of flatfoot deformity.
Yes, flatfoot deformity can have a familial connection. Individuals with a family history of flatfoot may be more susceptible to developing the condition. However, environmental factors, such as obesity and footwear choices, also contribute to the severity and progression of flatfoot deformity.
Non-surgical treatments for flatfoot deformity aim to alleviate symptoms and improve foot function. My approach to non-surgical treatments includes:
- Orthotic Devices: Custom-made or over-the-counter arch supports to provide additional support and redistribute pressure.
- Footwear Modifications: Choosing supportive shoes with good arch support and a firm heel counter.
- Physical Therapy: Specific exercises to strengthen the muscles and improve flexibility in the foot.
- Weight Management: Maintaining a healthy weight to reduce stress on the feet.
- Bracing: Using ankle braces or splints to provide additional support.
Early intervention with these measures can effectively manage flatfoot deformity and enhance overall foot comfort.
When non-surgical methods prove insufficient, surgical intervention may be considered. Common surgical procedures for flatfoot deformity include:
- Tendon Transfer: Repositioning tendons to support the arch.
- Osteotomy: Cutting and realigning bones to correct the arch.
- Arthrodesis: Fusing joints to provide stability.
- Implants: Inserting devices to support the arch.
The choice of surgery depends on the severity of the flatfoot deformity and the underlying causes.
Posterior tibial tendon dysfunction (PTTD) is a major contributor to the development of flatfoot deformity. The posterior tibial tendon plays a crucial role in supporting the arch and preventing it from collapsing. When this tendon weakens or becomes damaged, it can result in a flatfoot deformity, leading to pain, swelling, and difficulty with walking.
Treatment of Posterior Tibial Tendon Dysfunction (PTTD) Stages:
- Stage I: Inflammation: Non-surgical approaches include rest, ice, anti-inflammatory medications, and orthotic devices to support the foot.
- Stage II: Tendon Dysfunction: In addition to the above, physical therapy is introduced to strengthen the muscles and improve tendon function.
- Stage III: Deformity: Bracing, orthotics, and supportive footwear are used to alleviate symptoms. Surgical options may be considered for severe cases.
- Stage IV: Arthritis: Surgical interventions such as joint fusion or tendon transfers may be recommended to address pain and deformity.
How Long Is Recovery After Flatfoot Surgery?
Recovery time after flatfoot surgery varies depending on the specific procedure performed. Generally, patients can expect:
- Immediate Postoperative Period: Non-weight-bearing or limited weight-bearing with the use of crutches. This usually lasts several weeks.
- Follow-Up Appointments: Regular check-ups to monitor healing progress and make necessary adjustments.
- Physical Therapy: A structured program to regain strength, flexibility, and functionality. This can last for a couple months if needed.
- Gradual Return to Activities: Resumption of normal activities under the guidance of the surgeon.
Complete recovery may take several months, with full return to regular activities occurring gradually as the foot heals and gains strength.
In the realm of flatfoot deformity, expert guidance and compassionate care are pivotal for successful management. As a foot surgeon dedicated to foot health, Dr. Golding advocates for early intervention, personalized treatment plans, and comprehensive postoperative care. Whether exploring non-surgical options or considering surgical intervention, rest assured that expert guidance is available to help you navigate the path to relief and improved foot health. Learn more about Dr. Stephanie Golding at Bone and Joint Specialists of Winchester today for expert care and effective treatments. Get back to walking comfortably and confidently!
 What is the Achilles tendon?
What is the Achilles tendon?
The Achilles tendon is a strong band of tissue that connects your calf muscles to your heel bone. It allows you to walk, run, and jump, but despite its strength, it's also prone to injury. At Bone and Joint Specialists of Winchester, we provide expert care for Achilles tendon issues, guided by the experienced Dr. Stephanie Golding.
Common Achilles Tendon Injuries
When the Achilles tendon is overly stressed or stretched beyond its capacity, injuries can occur. Dr. Stephanie Golding and the team at Bone and Joint Specialists of Winchester diagnose and treat a wide range of Achilles tendon injuries, including:
- Achilles Tendonitis
- Non-Insertional Achilles Tendonitis: This involves small tears in the middle fibers of the tendon, causing pain and swelling.
- Insertional Achilles Tendonitis: This occurs where the Achilles tendon meets your heel bone and can lead to the development of bone spurs.
- Achilles Rupture
- Severe tears in the tendon fibers can lead to a complete or partial rupture. This serious injury requires immediate medical attention as it involves the tendon fibers completely severing.
PARS Minimally Invasive Achilles Repair
The PARS (Percutaneous Achilles Repair System) technique is a new, minimally invasive method for Achilles tendon repair. This approach uses a smaller 1-2 cm incision compared to the traditional 10-15 cm incision. Benefits include less swelling and scar tissue formation, allowing for a quicker recovery. Dr. Stephanie Golding and the surgical team at Bone and Joint Specialists of Winchester use this technique to help patients recover faster.
Symptoms of an Achilles Tendon Injury
A complete Achilles rupture causes sudden, intense pain at the back of your ankle and lower leg, often accompanied by a popping or snapping noise. Achilles tendonitis, though less severe, still causes significant discomfort with symptoms including:
- Thickening of the tendon
- Swelling and stiffness
- Difficulty walking on the injured leg
- Bone spurs on the heel
Without treatment, Achilles tendonitis can worsen and become a chronic condition.
Diagnosis and Treatment of Achilles Tendon Injuries
Dr. Stephanie Golding and her team at Bone and Joint Specialists of Winchester begin with a careful examination of your foot, along with a review of your symptoms and medical history. Diagnostic tools like ultrasound or MRI scans may be used to assess the extent of the injury.
Treatment options for Achilles tendon injuries include:
- Rest, ice, compression, and elevation (RICE)
- Physical therapy
- Pain-relieving medications
- Custom orthotics
If non-surgical treatments are ineffective, regenerative medicine options like platelet-rich plasma (PRP) or stem cell injections may be recommended. In cases where the Achilles tendon is torn, surgery may be necessary. Dr. Stephanie Golding specializes in minimally invasive procedures to ensure the best outcomes for her patients.
Call Bone and Joint Specialists of Winchester at the first sign of an Achilles tendon tear, or request an appointment online today. Dr. Stephanie Golding and her team are dedicated to providing expert care for all your foot and ankle needs.
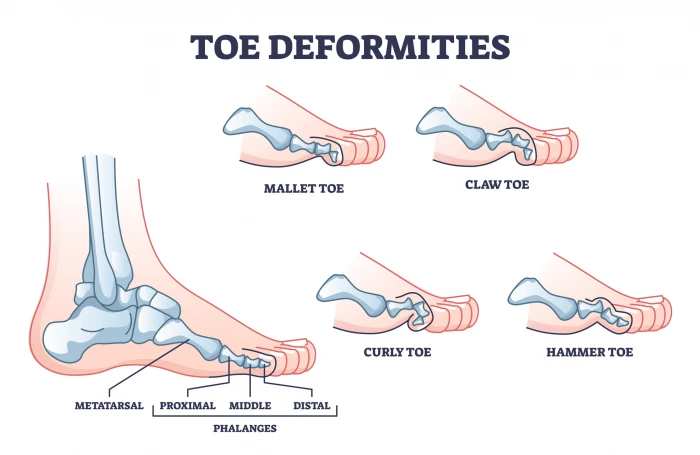 What are Hammer, Claw, and Mallet Toes?
What are Hammer, Claw, and Mallet Toes?
Hammer, claw, and mallet toes are toe deformities where the toes are bent into unusual positions. These conditions usually affect the four smaller toes, not the big toe. They can look strange and may hurt.
- Hammer Toe: This occurs when the middle joint of a toe bends down toward the floor, causing the middle joint to rise up. It typically affects the second toe and often occurs alongside bunions.
- Claw Toe: This affects the four smaller toes at the same time. The toes bend up at the joint where they meet the foot, and down at the middle joints and the joints nearest the tip, making the toes curl toward the floor.
- Mallet Toe: This involves a downward bend at the joint closest to the tip of the toe, often affecting the second toe but can occur in other toes as well.
If you notice your toe looks odd or hurts, consult Dr. Stephanie Golding at Bone and Joint Specialists of Winchester. Early treatment can often fix the problem without surgery.
What Causes Them?
The most common cause of these toe problems is wearing tight shoes. Tight shoes can force the toes into bent positions, causing muscle imbalance and tendon shortening. Over time, this makes it harder to straighten the toes even when not wearing shoes.
These conditions develop over many years and are more common in adults. Women are more frequently affected than men due to the likelihood of wearing narrow-toed or high-heeled shoes. Less commonly, these problems can be linked to other conditions like diabetes, rheumatoid arthritis, stroke, or foot and ankle injuries.
What Are the Symptoms?
Hammer, claw, and mallet toes can cause pain and make it difficult to find comfortable shoes. The affected toes may rub against footwear, leading to calluses or corns. In severe cases, these deformities can affect balance and walking.
How Are They Diagnosed?
Dr. Stephanie Golding will ask about your symptoms, medical history, and footwear habits during the physical exam. She'll want to know:
- When the problems started and what makes them worse.
- The type of shoes you wear and how much time you spend standing or walking daily.
- Any previous foot problems and related medical conditions such as arthritis, diabetes, or poor blood circulation.
During the exam, Dr. Golding will check if the toe joints are flexible or fixed. Flexible joints can sometimes be straightened without surgery, while fixed joints often require surgical intervention. If surgery might be needed, tests like X-rays, blood flow tests, or nerve tests may be conducted.
How Can You Care for Yourself at Home?
You can manage many toe joint problems at home. Early treatment can prevent the need for surgery.
- Change Your Footwear: Choose shoes with roomy toe boxes, low heels, and good arch support. Sandals or athletic shoes that don't rub on your toes are good options. Consider custom-made shoes for specific foot problems.
- Use Cushions and Supports: Products like moleskin, toe tubes, arch supports, or other shoe inserts can cushion the toe or hold the foot in a more comfortable position, especially for flexible toes.
- Care for Calluses and Corns: Use over-the-counter treatments to relieve pain. Never cut corns or calluses as this can lead to infection.
- Pain Relief: Take over-the-counter pain medications like acetaminophen, ibuprofen, or naproxen. Always follow the instructions on the label and consult your doctor.
If your toe joint is flexible, additional treatments include:
- Taping a Hammer Toe: Wrap tape under the big toe, then over the hammer toe, and under the next toe to gently force the hammer toe into a normal position temporarily.
- Toe Caps, Slings, or Splints: These hold toes in a normal position, similar to taping.
- Exercises: Strengthen and keep the toe joints flexible. Examples include gently stretching bent joints, towel scrunches (using your toes to crumple a towel), and marble pickups (using your toes to pick up marbles and drop them into a cup).
How Are These Toe Problems Treated?
Surgery might be necessary if other treatments don't relieve pain, if the toe limits activity, or if you can't move the joint (fixed toe problem). Surgery is generally reserved for severe cases.
- For Fixed Toe Problems: Surgery often involves working on the bones. Options include removing part of the toe bone or part of the joint and letting the bones grow together.
- For Flexible Toe Problems: Surgery may involve moving tendons to release tension on the joint, allowing the toe to straighten. Sometimes, bone work is also necessary.
Dr. Stephanie Golding will discuss your options and their potential benefits with you. If you're experiencing toe problems, contact Dr. Stephanie Golding at Bone and Joint Specialists of Winchester for expert care and guidance.
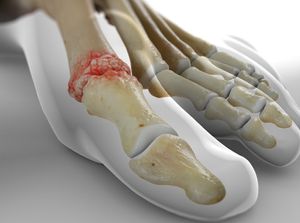
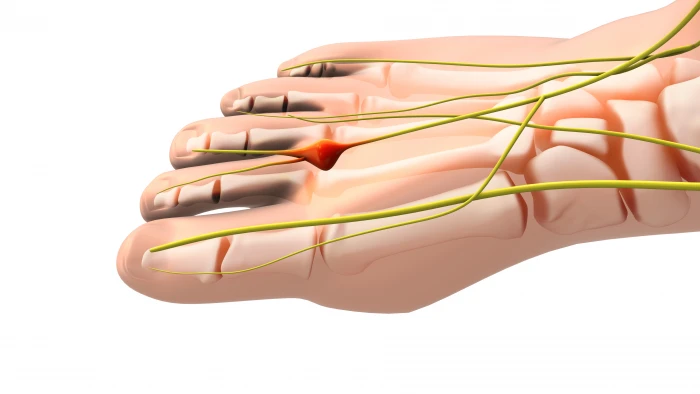 Do you feel like there is a pebble under the ball of your foot? Do you get burning pain or tingling of your toes? Then you may have a Morton’s neuroma. Morton's neuroma is a painful condition affecting the ball of your foot, often between the third and fourth toes. Dr. Stephanie Golding at Bone and Joint Specialists of Winchester is here to help you understand and treat this condition.
Do you feel like there is a pebble under the ball of your foot? Do you get burning pain or tingling of your toes? Then you may have a Morton’s neuroma. Morton's neuroma is a painful condition affecting the ball of your foot, often between the third and fourth toes. Dr. Stephanie Golding at Bone and Joint Specialists of Winchester is here to help you understand and treat this condition.
Signs and Symptoms
Morton's neuroma happens when a nerve in your foot becomes swollen and irritated. Common signs include:
- A sharp, burning pain in the ball of your foot
- Tingling or numbness in your toes
- Feeling like there's a pebble in your shoe
These symptoms can worsen with tight shoes or activities like running.
Causes
Morton's neuroma is often caused by wearing tight or high-heeled shoes. These shoes put pressure on the nerves in your feet. Other causes include high-impact activities and foot deformities like bunions or flat feet.
Treatments
Dr. Stephanie Golding at Bone and Joint Specialists of Winchester offers various treatments to help relieve the pain of Morton's neuroma:
- Footwear Changes: Wear shoes with a wider toe box and low heels. This reduces pressure on your foot.
- Padding and Orthotics: Special pads and custom shoe inserts can help support your foot and reduce pain.
- Medications: Over-the-counter pain relievers and anti-inflammatory medications can help.
- Injections: Corticosteroid injections can reduce swelling and pain.
- Physical Therapy: Exercises and massages can help improve foot function.
- Surgery: In severe cases, surgery may be needed to remove the damaged nerve.
If you experience symptoms of Morton's neuroma, contact Dr. Stephanie Golding at Bone and Joint Specialists of Winchester for expert care and treatment. Early intervention can help you get back on your feet and enjoy your daily activities.
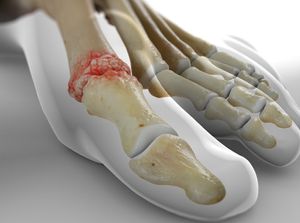
 Do you have foot arthritis?
Do you have foot arthritis?
Arthritis can affect the feet and ankles just like any other joint. It can cause pain, stiffness, and deformity. The most common type is osteoarthritis, which involves the wearing down of joint cartilage. Rheumatoid arthritis and arthritis after fractures also frequently affect the feet. At Bone and Joint Specialists of Winchester, Dr. Stephanie Golding is here to help you manage and treat foot arthritis.
Diagnosing Foot Arthritis
Dr. Stephanie Golding can accurately diagnose the type of arthritis affecting your feet and ankles. The evaluation process includes:
- Taking a detailed medical history
- Checking your range of motion
- Evaluating the alignment of your feet and ankles
- Feeling for tenderness in the joints
Additionally, Dr. Golding will observe how you move and may take X-rays or perform other necessary tests. Once diagnosed, she will create a personalized treatment plan for you.
Treatment Options
Dr. Golding offers various treatments to reduce pain and inflammation caused by foot arthritis, including:
Medication:
- Non-steroidal anti-inflammatory drugs (NSAIDs) to reduce inflammation and pain
- Corticosteroids or disease-modifying anti-rheumatic drugs (DMARDs) for more severe cases
Physical Therapy:
- Exercises to improve movement and increase the range of motion
- Cold and hot compresses to reduce pain and swelling
Custom Orthotics:
- Specialized devices fitted in your shoes to support your feet
- Reduce pressure on arthritic joints
- Improve gait mechanics and relieve discomfort
Surgery: In severe cases, Dr. Golding may recommend surgery, such as joint fusion or arthrodesis, to reduce pain and improve joint stability.
Foot Care Advice
Proper foot care is essential for managing foot arthritis. Dr. Golding provides valuable advice, including:
- Choosing shoes that fit well and support your feet
- Keeping your feet clean and dry
- Protecting your feet from injuries
- Doing regular exercises
- Eating a balanced diet
- Limiting activities that strain your feet and ankles
Being attentive to your foot care can prevent the condition from worsening.
When to Visit Dr. Golding
If you experience pain, stiffness, or swelling in your feet and ankles, it’s important to visit Dr. Stephanie Golding at Bone and Joint Specialists of Winchester. Early diagnosis and treatment can prevent the condition from worsening. Dr. Golding will recommend a treatment plan tailored to your needs, helping you manage your foot arthritis and improve your quality of life.
Why Choose Dr. Stephanie Golding for Foot Arthritis
Dr. Stephanie Golding specializes in diagnosing and treating foot and ankle conditions. She has the expertise to accurately evaluate your condition and recommend a course of treatment tailored to your needs. In addition to providing relief from pain and inflammation, Dr. Golding focuses on preventive care, helping you manage your foot arthritis and prevent it from worsening.
If you're suffering from foot arthritis, contact Dr. Stephanie Golding at Bone and Joint Specialists of Winchester. She will take the time to understand your condition and create a plan that works for you.
 What is Tarsal Tunnel Syndrome?
What is Tarsal Tunnel Syndrome?
Do you feel tingling, burning, or numbness in your foot? Do you have pain that spreads from your ankle into your toes? These could be signs of tarsal tunnel syndrome. Dr. Stephanie Golding at Bone and Joint Specialists of Winchester is here to help you understand and treat this condition.
What is Tarsal Tunnel Syndrome?
Tarsal tunnel syndrome is a condition where the tibial nerve, which runs through a narrow tunnel in your ankle, gets compressed. This tunnel is called the tarsal tunnel. When the nerve is squeezed, it causes pain and other symptoms in your foot.
Symptoms of Tarsal Tunnel Syndrome
Common signs of tarsal tunnel syndrome include:
- Tingling or numbness in the bottom of your foot and toes
- A burning sensation in your foot
- Sharp or shooting pain that starts in your ankle and moves to your toes
- Swelling in your foot
These symptoms can worsen with activity and may feel better with rest.
Causes of Tarsal Tunnel Syndrome
Several things can cause tarsal tunnel syndrome, including:
- Injury to the ankle
- Swelling from conditions like arthritis
- Diabetes, which can affect nerve function
- Flat feet, which can stretch the tibial nerve
Treatments for Tarsal Tunnel Syndrome
Dr. Stephanie Golding at Bone and Joint Specialists of Winchester offers several treatments to help relieve the pain and discomfort of tarsal tunnel syndrome:
- Rest and Ice: Resting your foot and applying ice can reduce swelling and pain.
- Medications: Over-the-counter pain relievers and anti-inflammatory drugs can help.
- Supportive Footwear: Wearing shoes with good arch support can ease pressure on the tibial nerve.
- Orthotics: Custom shoe inserts can provide additional support and reduce symptoms.
- Physical Therapy: Exercises can strengthen your foot and ankle, improving flexibility and reducing nerve compression.
- Injections: Corticosteroid injections can reduce inflammation and relieve pain.
- Surgery: In severe cases, surgery may be needed to release the pressure on the nerve.
If you think you might have tarsal tunnel syndrome, contact Dr. Stephanie Golding at Bone and Joint Specialists of Winchester. Early treatment can help reduce symptoms and improve your quality of life. Don't let foot pain hold you back – get the care you need today!
 What is Posterior Tibial Tendonitis?
What is Posterior Tibial Tendonitis?
Do you feel pain or swelling along the inside of your ankle? Does your foot feel weak or unstable when you walk? These could be signs of posterior tibial tendonitis. Dr. Stephanie Golding at Bone and Joint Specialists of Winchester is here to help you understand and treat this condition.
What is Posterior Tibial Tendonitis?
Posterior tibial tendonitis is a condition where the posterior tibial tendon, which runs along the inside of your ankle, becomes inflamed or torn. This tendon helps support the arch of your foot and is important for walking. When it gets damaged, it can cause pain and difficulty with walking.
Symptoms of Posterior Tibial Tendonitis
Common signs of posterior tibial tendonitis include:
- Pain and swelling along the inside of the ankle
- Pain that worsens with activity
- A flattening of the arch of the foot
- Weakness or instability in the foot and ankle
These symptoms can make walking difficult and uncomfortable.
Causes of Posterior Tibial Tendonitis
Several factors can cause posterior tibial tendonitis, including:
- Overuse from activities like running or walking
- Foot deformities, such as flat feet
- An injury to the foot or ankle
- Conditions like arthritis that affect the joints
Treatments for Posterior Tibial Tendonitis
Dr. Stephanie Golding at Bone and Joint Specialists of Winchester offers several treatments to help relieve the pain and discomfort of posterior tibial tendonitis:
- Rest and Ice: Resting your foot and applying ice can reduce swelling and pain.
- Medications: Over-the-counter pain relievers and anti-inflammatory drugs can help.
- Supportive Footwear: Wearing shoes with good arch support can ease pressure on the tendon.
- Orthotics: Custom shoe inserts can provide additional support and reduce symptoms.
- Physical Therapy: Exercises can strengthen your foot and ankle, improving flexibility and reducing inflammation.
- Surgery: In severe cases, surgery may be needed to repair the tendon.
If you think you might have posterior tibial tendonitis, contact Dr. Stephanie Golding at Bone and Joint Specialists of Winchester. Early treatment can help reduce symptoms and improve your quality of life. Don’t let foot pain hold you back – get the care you need today!
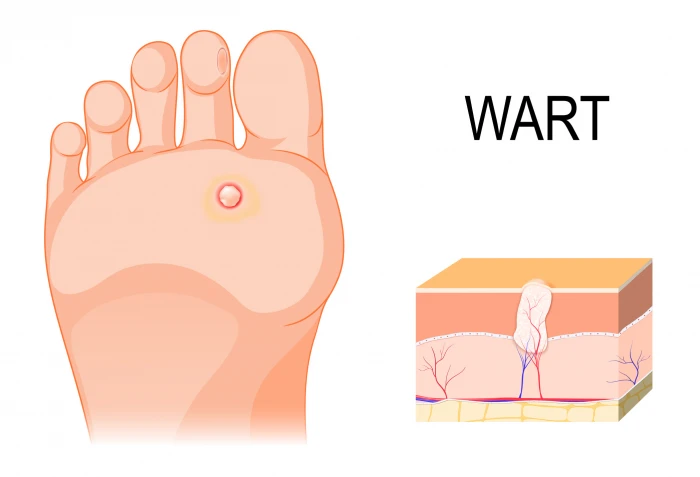 Treating Warts on Feet and Toes
Treating Warts on Feet and Toes
Do you have painful or unsightly warts on your feet? Dr. Stephanie Golding at Bone and Joint Specialists of Winchester can help. Foot warts are common and can cause discomfort. There are several types of warts and effective treatments available.
The most common type of wart is a plantar wart. Plantar warts appear on the soles of your feet and can be painful, especially when walking. They often have black dots in the center, which are tiny blood vessels.
Common Treatments:
Dr. Golding offers several treatments to remove foot warts and relieve pain:
- Topical Treatments: Special creams and solutions can be applied directly to the wart to help dissolve it over time.
- Cryotherapy: This involves freezing the wart with liquid nitrogen, causing it to fall off.
- Laser Therapy: A laser can target and destroy the wart tissue.
- Surgical Removal: In stubborn cases, the wart can be surgically removed.
If you have warts on your feet, don't let them cause you pain or embarrassment. Contact Dr. Stephanie Golding at Bone and Joint Specialists of Winchester today for expert care and effective treatments. Get back to walking comfortably and confidently!
 Understanding and Treating Ingrown Toenails
Understanding and Treating Ingrown Toenails
Ingrown toenails can be a painful and bothersome condition. If you're experiencing discomfort from an ingrown toenail, Dr. Stephanie Golding at Bone and Joint Specialists of Winchester can help.
What Are Ingrown Toenails?
An ingrown toenail occurs when the edge of the toenail grows into the skin surrounding it. This can cause pain, redness, swelling, and sometimes infection. The big toe is most commonly affected, but any toenail can become ingrown.
Causes of Ingrown Toenails
Several factors can lead to ingrown toenails, including:
- Improper Nail Trimming: Cutting nails too short or rounding the edges can encourage the nail to grow into the skin.
- Tight Footwear: Shoes that are too tight can put pressure on the toes, causing the nail to grow inward.
- Injury: Trauma to the toe, such as stubbing it or having it stepped on, can lead to an ingrown nail.
- Genetics: Some people are more prone to ingrown toenails due to the natural shape and thickness of their nails.
Treatment Options
Dr. Golding offers several effective treatments for ingrown toenails at Bone and Joint Specialists of Winchester:
- Home Care: Soaking the affected foot in warm water several times a day can help reduce swelling and relieve pain. Gently lifting the nail edge can help guide the nail to grow above the skin.
- Medications: Over-the-counter pain relievers and topical antibiotics can help manage pain and prevent infection.
- Nail Trimming: Dr. Golding can carefully trim the ingrown portion of the nail to provide immediate relief.
- Partial Nail Removal: In more severe cases, removing part of the nail and the underlying tissue can prevent the nail from growing back ingrown.
- Complete Nail Removal: For recurrent ingrown nails, the entire nail may be removed. This is usually a last resort and is not always a permanent procedure, allowing the nail to possibly grow back normally.
If you are suffering from an ingrown toenail, don't wait for the pain to worsen. Contact Dr. Golding at Bone and Joint Specialists of Winchester for expert care and effective treatments. Get back to enjoying pain-free steps today!
Finding Relief from Fallen Arches: Expert Care with Dr. Stephanie Golding
Do you experience foot pain or discomfort while walking? You might have fallen arches, also known as flat feet. Dr. Stephanie Golding at Bone and Joint Specialists of Winchester is here to help you understand and treat this condition.
What Are Fallen Arches?
Fallen arches occur when the arch of the foot collapses, causing the entire sole to touch the ground. This condition can lead to foot pain, swelling, and difficulty walking. Flat feet can be present from birth or develop over time due to injury or wear and tear.
Causes of Fallen Arches
Several factors can contribute to fallen arches, including:
- Genetics: Some people are born with flat feet.
- Injury: Foot or ankle injuries can weaken the tendons and muscles, leading to fallen arches.
- Aging: As we age, the posterior tibial tendon can weaken, resulting in fallen arches.
- Obesity: Excess weight puts extra strain on the feet, contributing to flat feet.
Symptoms of Fallen Arches
Common symptoms of fallen arches include:
- Foot pain, especially in the arch or heel
- Swelling along the inside of the ankle
- Difficulty standing on tiptoes
- Flat appearance of the foot
Treatment Options
Dr. Golding offers several treatments for fallen arches at Bone and Joint Specialists of Winchester:
- Orthotics: Custom shoe inserts can provide support and relieve pain by improving foot alignment.
- Supportive Footwear: Wearing shoes with good arch support and a firm heel can help manage symptoms.
- Physical Therapy: Exercises can strengthen the muscles and tendons in the feet, improving arch support.
- Medications: Over-the-counter pain relievers and anti-inflammatory medications can help manage pain and swelling.
- Surgery: In severe cases, surgery may be necessary to correct the arch and relieve symptoms.
If you think you might have fallen arches, contact Dr. Stephanie Golding at Bone and Joint Specialists of Winchester. Early treatment can help reduce pain and improve your quality of life. Don't let foot pain hold you back – get the expert care you need today!
Videos
-
 ProcedureAnkle Fracture Surgery
ProcedureAnkle Fracture Surgery -
 ProcedureAnkle Replacement
ProcedureAnkle Replacement -
 ProcedureBunionectomy (Chevron Bunionectomy)
ProcedureBunionectomy (Chevron Bunionectomy) -
 ProcedureCheilectomy
ProcedureCheilectomy -
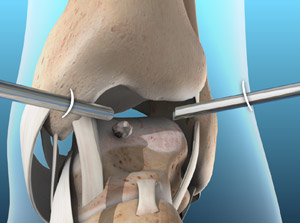 ProcedureArthroscopy of the Ankle
ProcedureArthroscopy of the Ankle -
 ConditionMorton's Neuroma
ConditionMorton's Neuroma -
 ProcedureHammertoe Correction (PIP Joint Arthroplasty)
ProcedureHammertoe Correction (PIP Joint Arthroplasty) -
 ProcedureLateral Ankle Ligament Reconstruction
ProcedureLateral Ankle Ligament Reconstruction -
 ConditionTarsal Tunnel Syndrome (Posterior Tibial Neuralgia)
ConditionTarsal Tunnel Syndrome (Posterior Tibial Neuralgia) -
 ConditionPosterior Tibial Tendon Dysfunction (PTTD)
ConditionPosterior Tibial Tendon Dysfunction (PTTD) -
 ConditionPlantar Warts
ConditionPlantar Warts -
 ConditionIngrown Toenails
ConditionIngrown Toenails